Background
As survival of preterm infants improves, attention is focused on improving the quality of survival through optimal nutrition management. Studies have shown that human milk (HM) is the best source of nutrition for preterm infants, conferring short and long-term health benefits, such as protecting against infections, particularly of the gut. HM contains hormones, nutrients and growth factors that help the preterm infant grow and develop. HM is not always available for every feeding, and there is no practical way to evaluate a high human milk diet versus a low human milk diet and the correlated outcomes.
Purpose
This work aimed to extract 5 years of feeding and nutrition data from the electronic health record (her) using secure Fast Healthcare Interoperability Resources Application Programming Interfaces (FHIR APIs), a standard for exchanging private health information. A proprietary nutrition IQ framework was applied to imported data to interpret and evaluate outcomes, growth metrics, and adherence to consensus-based enteral feeding protocols.
Methods
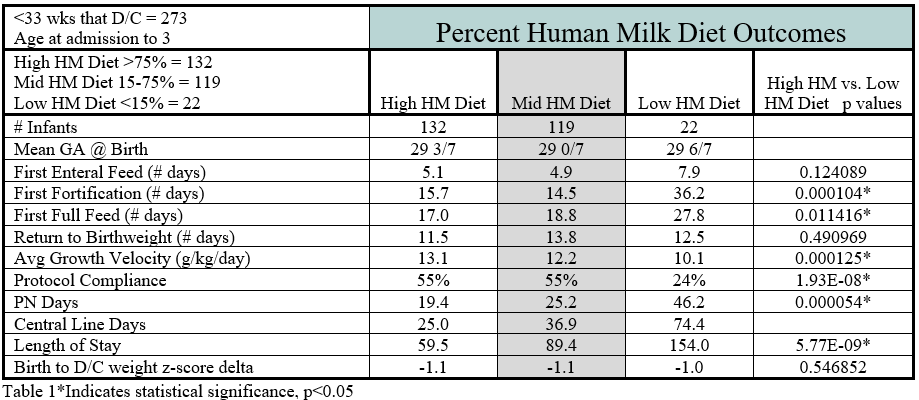
Inclusion criteria of admission by 3 days and <33 weeks estimated gestational age (EGA) that subsequently discharged from NICU identified 273 infants. 3 cohorts based on the percentage of their enteral diet that came from HM were created. Cohort 1 “High HM Diet” – diet contained more than 75% HM (132), cohort 2 “Mid HM Diet” – diet contained 15% to 75% HM (119), and cohort 3 “Low HM Diet” –diet contained less than 15% HM (22).
Results
Comparing cohort 1 to cohort 3 showed a trend toward improvement in earlier initiation of enteral feeding and return to birthweight (RTBW). Cohort 1 demonstrated clinically and statistically increased growth velocity (13.1g/d vs 10.1g/d), a decrease in days to fortification (15.7 vs 36.1) and first full feed (17 vs 27.8). Protocol adherence was significantly better in cohort 1 versus cohort 3 (55% vs 24%). Days on parenteral nutrition (PN) (19.4 vs 46.2), central line days (25.0 vs 74.4), and length of stay (59.5 vs 154) were less in cohort 1 compared to cohort 3 (Table 1).
Conclusion
Preterm infants receiving high HM diets are significantly more likely to remain on track with feeding protocols and reach fortification and full enteral feeding faster decreasing the risk associated with prolonged PN requirement and more days requiring a central line. This outcome is most likely associated with improved feeding tolerance and lower occurrence of adverse events which would prolong time on PN, days with a central line, and would delay achievement of full enteral feeds. Low HM diet infants had substantially longer hospitalization likely as a consequence of the occurrence of comorbidities that occur with less frequency in a high HM diet. This dose dependent effect of percent human milk in the diet on preterm infant outcomes has been discussed elsewhere in the medical literature and further investigation on the optimal dose of HM, length of exposure to HM and source of HM would further understanding of preterm nutritional needs.
Nicholas Rowley1, Dave Genetti2, Tammi Jantzen2, Laura Carroll1, Misty Virmani1
1Department of Pediatrics, University of Arkansas for Medical Sciences, 2Astarte Medical