By: William Hay, Jr., MD, Chief Medical Officer

Why is growth important?
Because it is THE unique characteristic of fetal and thus preterm infant life. It is what the fetus, and thus the preterm infant, must do in order to survive and to develop into a healthy, capable child and adult. The American Academy of Pediatrics has stated (AAP, Pediatric Nutrition 8th Ed. 2019), “Current recommendations for parenteral and enteral nutrition for very preterm infants are designed to provide nutrients to approximate the rate of growth and composition of weight gain for a normal fetus of the same postmenstrual age, and to maintain normal concentrations of blood and tissue nutrients.”
If growth is so important, why don’t preterm infants always grow as the normal fetus does?
A principal reason—inadequate nutrition—as evidenced by cumulative deficits in energy and protein, even with more “aggressive” or more “optimal” nutrition among a great many, apparently the majority, of preterm infants. Historically, there have been several common causes of inadequate nutrition of preterm infants:
- Delayed start to providing nutrients
Intravenous amino acids often have not been given on day 1 to sometimes several days after birth, and then are only started at very low rates, e.g., < 1.5 g/kg/day. Similarly, enteral feedings often have been withheld, sometimes for days, and then only started at very low rates, e.g., 12 cc/kg/d (2 cc/kg/4 hrs).
- Slow advances of nutrient supplies
Even after starting IV amino acids, they have been advanced slowly, e.g., 0.5 g/kg/d per day or even every other day. And similarly, enteral feeds often have been advanced slowly, e.g., 18-24 ml/kg/day.
- Dilute nutritional mixes
Frequently, preterm infants have been fed unfortified breast milk (mother’s own or banked) at slow rates, and intravenous amino acid mixtures can have insufficient amounts of essential amino acids, which will limit growth.
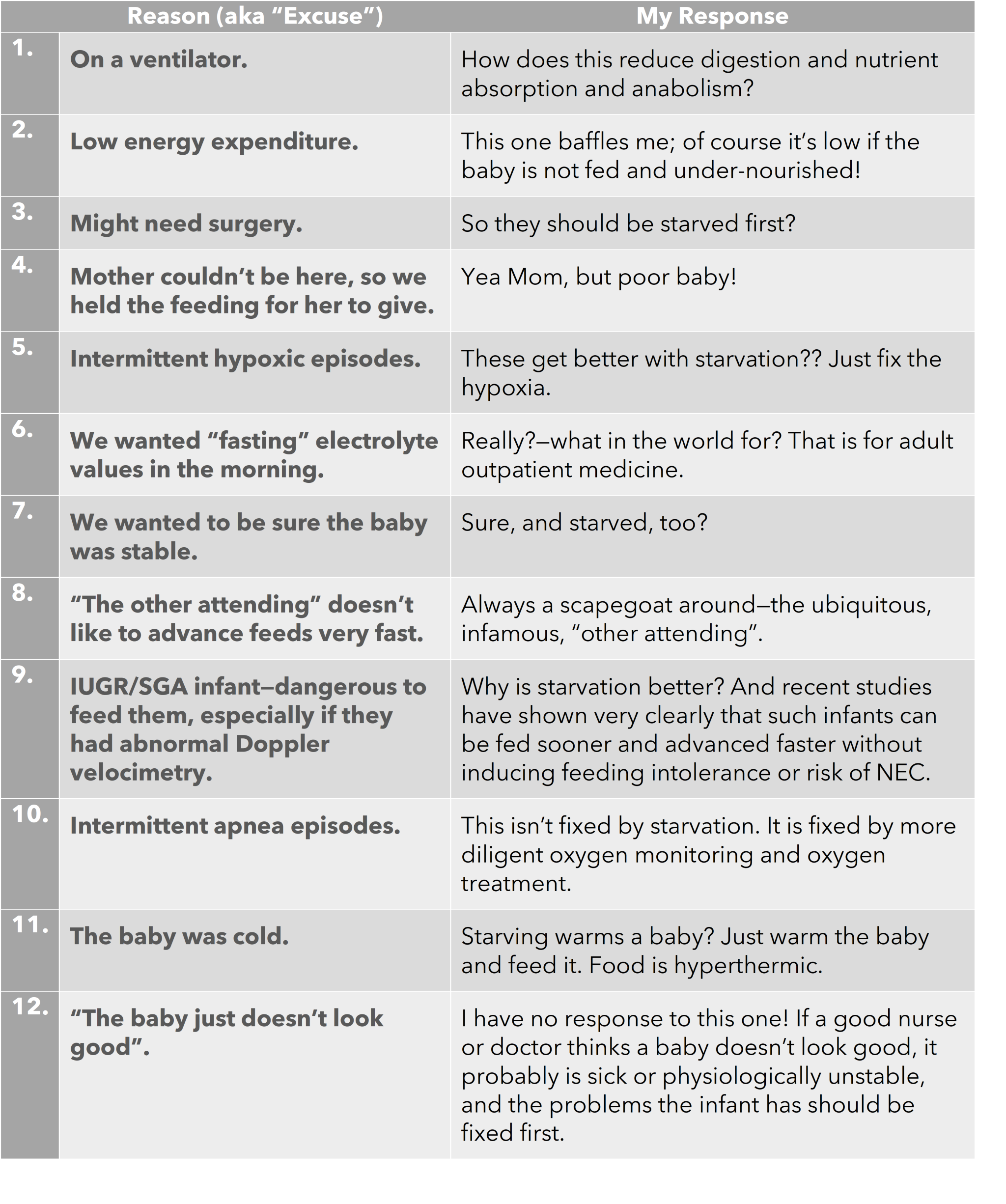
And there are many more–!! The reasons (“excuses”) seem never ending. The point is, though–all of these excuses, justified or not, reduce nutrient intake at critical stages of development, which limits growth with increased potential for long-lasting adverse outcomes.
One simply cannot say that factors other than under nutrition (e.g., many illnesses and pathophysiological processes and their treatments) are responsible for inadequate growth until one has provided appropriate and sufficient nutrition to meet the nutrient requirements of the preterm infant that match those of the normally growing human fetus.
Dr. William W. Hay, Jr. served as Professor of Pediatrics (Neonatology) at the University of Colorado Denver (retired). He was Head of the Section of Neonatology from 1982-1992 and Director of the ACGME/RRC accredited Training Program in Neonatal-Perinatal Medicine from 1982 until 2003. He also served as Director of the Child Maternal Health Program, now the Early Life Exposures Program and was Director for 36 years of the Neonatal-Perinatal Clinical Translational Research Center, for the NIH-NCATS-Colorado Clinical and Translational Sciences Institute. Dr. Hay’s principal administrative role was Scientific Director of the UCDenver–Department of Pediatrics/Section of Neonatology Perinatal Research Center. He is principal investigator and program director for an NIH-NICHD T32 Training Grant in Perinatal Biology and Medicine. Dr. Hay is widely published, with his research and scholarship appearing in more than 400 articles and books.