Background
Optimal nutrition management of preterm infants improves outcomes. Consensus-based feeding protocols provide evidence-based care with less variability and reduce adverse outcomes such as necrotizing enterocolitis (NEC). Digital tools that harness data from the EHR for monitoring and reporting on preterm infant feeding, nutrition, protocol adherence, and associated clinical outcomes are urgently needed.
Purpose
This work aimed to develop a .NET application to extract data directly from the EHR using secure Fast Healthcare Interoperability Resources Application Programming Interfaces (FHIR APIs), a standard for exchanging private health information. JavaScript frameworks were used to interpret and present data in an intuitive, user-friendly display. A proprietary Nutrition IQ framework was applied to incorporate three complex feeding protocols into the software application and 5 years of data extracted.
Methods
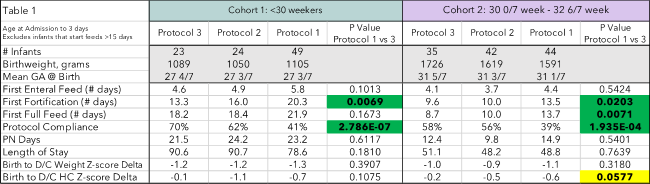
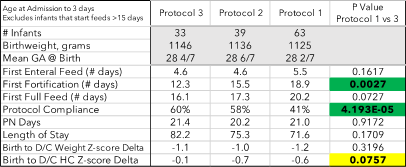
Inclusion criteria of admission before 3 days and <38 weeks estimated gestational age (EGA) identified 617 infants. Infants whose feeds initiated at 15 days or more were excluded from data analysis to account for surgical diagnoses (19). 227 unique individuals were placed in 3 cohorts. Cohort 1- infants born <30-week gestation (96), cohort 2 – EGA 30 0/7 to 32 6/7 (121), and cohort 3 – birthweight <1500g (135).
Three feeding protocols with successive implementation were analyzed for protocol adherence and outcomes. Feeding protocol 1 is a weight-based feeding advancement algorithm with two step fortification using a bovine-based human milk fortifier (bHMF) to 22 then 24 kcal/oz. In feeding protocol 2 the trophic feeding period was shortened from 5 to 3 days, feeding volume advanced faster, and single step fortification to 24kcal/oz using bHMF. In feeding protocol 3, infants born under 1250 grams were fortified with human milk based HMF with advancement to goal 26kcal/oz.
Results
Baseline characteristics of cohort subgroups did not statistically differ. Comparing protocol 1 to 3 showed a statistically and clinically significant decrease in days until the first fortification in all cohorts (Tables 1, 2). Days on parenteral nutrition (PN) trended towards a decrease in cohorts 1&2 (Table 1) but unchanged in cohort 3. Time to full enteral feeding volume decreased in all cohorts from protocol 1 to 3, reaching statistical significance in cohort 1 (Table 1) and approaching significance in cohort 3 (Table 2). Compliance with feeding protocols increased steadily across the feeding protocols reaching statistical significance in all groups (Tables 1 and 2).
NEC was identified as a potential adverse outcome measure to alterations in feeding protocols. Data for NEC from 2017-2020 for cohort 3 (2.7-5.7%) did not differ between protocols 1, 2 or 3. NEC rates during the EHMD protocol were lower than previous years recorded (1.7%) but the period and number of patients with NEC are too few to establish a correlation with the EHMD protocol.
Conclusion
The current ability to measure the effectiveness of enteral feeding protocols is costly and time prohibitive. Implementing software that harnesses the data entered into the EHR, allows for real-time monitoring of protocol adherence and patient outcomes, enabling clinical teams to continuously educate staff and make adjustments to improve patient outcomes.
Misty Virmani1, Dave Genetti2, Aamir Nayeem2, Tammi Jantzen2,
Ashley Ross1, Laura Carroll1
1Department of Pediatrics, University of Arkansas for Medical Sciences, 2Astarte Medical